Human
A&P II – The cardiovascular system: THE HEART
I. Heart Anatomy
A.
Size, Location, & Orientation
1. Situated between the lungs in the
_____________________
with 2/3 of its mass to
the left of the midline
2. About the size of a clenched fist, hollow,
& cone-shaped;
weighing
_____________________ (less than one pound)
3. Rests on the superior surface of
_____________________,
flanked laterally by
_____________________ which partially
obscure it. Lies between the vertebral column & the
sternum (two
rigid structures)
4. _____________________ is directed toward the
right shoulder
& the
_____________________ points toward the left hip
B.
Covering the Heart:
_____________________ – a double-walled sac
1. _____________________ pericardium – tough, connective
tissue layer with 3
functions
a. Protects the heart
b. Anchors it to surrounding structures like
diaphragm &
great
vessels
c. Prevents overfilling of the heart w/blood
2. _____________________ pericardium – composed of a
parietal layer & a
visceral layer
a. _____________________ layer – lines the internal
surface of
the fibrous pericardium
b. _____________________ layer or
_____________________
(“upon the heart”) – covers
the
external heart surface & forms the exterior layer of the
heart’s wall
3. Pericardial
cavity – between the parietal & visceral layers of
the serous pericardium
is a potential space filled with
_____________________________
that reduces friction between
the two membranes.
a. _____________________ – inflammation of the
pericardium
that reduces fluid production & causes friction
due to
rubbing. Can lead to adhesions in which
the two
layers stick
together & impede heart function.
b. ______________________________ – Fluid seeps
into
cavity and
compresses the heart.
C.
Layers of the Heart Wall – the heart wall has 3 layers
1. _____________________ – outermost layer,
composed of
mesothelium and
connective tissue
2. _____________________ – primarily cardiac muscle.
Forms
the bulk of the heart
& is the layer that actually contracts.
a. Muscle fibers are organized in a spiral
around the heart
1) Fibers are striated, involuntary, &
interconnected
by branching networks connected by
 _____________________
_____________________
b. __________________________________ –
connective
tissue fibers form a dense network of collagen & elastin to support &
anchor cardiac muscle.
1) Foundation to which the
heart valves
attach
2) Serves as points of
insertion for
cardiac muscle bundles
3) Prevents
overstretching of the valves
as blood passes through
them
4) Acts as an electrical
insulator that
prevents direct spread of
action
potentials from the
atria to the
ventricles (in other
words, it is not
electrically excitable)
3. _____________________ (“inside the heart”) –
consists of
squamous epithelium
& connective tissue
a. Lines the heart chambers & is continuous
w/endothelial
linings of
great blood vessels.
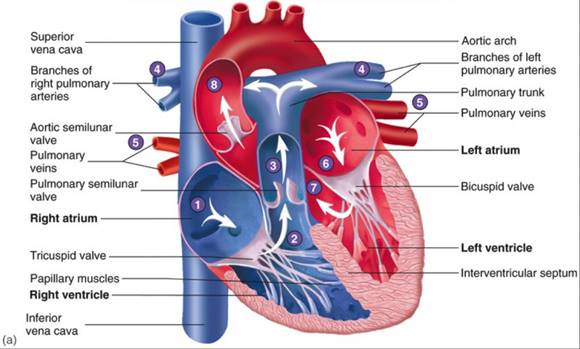
D. Chambers of the Heart
1. The chambers include 2 superior _____________________
& 2
inferior
_____________________
a. Atria
(“entry way”) are receiving chambers for blood
returning to the heart from
circulation
1)
chambers are divided longitudinally by
_____________________
2)
septum has an oval depression, the fossa
ovalis,
which
is the remnant of the foramen ovale
b. Ventricles
– discharging chambers of the heart
1)
chambers are divided longitudinally
_____________________
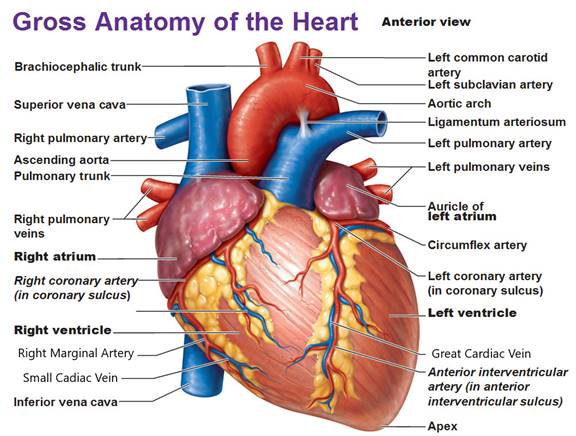
2. On the surface of the heart are the auricles
& sulci
a. The _____________________ are small pouches
on the
anterior
surface of each atrium (they look like small external
flaps) that
slightly increase the capacity of each atrium.
b. The _____________________ are grooves that
contain
blood
vessels & fat & separate the chambers
3. Right
atrium
a. Receives oxygen-poor blood from 3 veins…
1) _______________________________________–
blood
from body regions superior to the diaphragm
2) _______________________________________ –
blood
from body regions below the diaphragm
3) _______________________________________ –
collects
blood draining from the myocardium itself
b. Blood passes from the rt. atrium into the rt.
ventricle
through the
_____________________
4. Right
ventricle
a. Forms most of the anterior surface of the
heart
b. Blood
passes from the rt. ventricle to the
________________________________
via the
__________________________________________
c.
Pulmonary trunk exits from the rt. side & goes to the
lungs
5. Left
atrium
a. Receives oxygen-rich blood from the pulmonary
veins
b. Blood passes from the lt. atrium to the lt.
ventricle through
the
_____________________
6. Left
ventricle
a. Forms the apex of the heart
b. Blood passes from the lt. ventricle through
the
__________________________________________
into the
_____________________.
c. Aorta exits from the lt. side and goes to the
rest of the
body
7. During fetal life the ductus arteriosus shunts blood from the
pulmonary trunk into the
aorta. At birth, the ductus arteriosus
closes & becomes the
ligamentum arteriosum.
E.
Myocardial thickness & function
1. Atria walls are thin because they deliver
blood to the ventricles
2. Ventricle walls are thicker because they pump
blood greater
distances
a. Rt. ventricle walls are thinner because they
pump blood
into the
lungs, which are nearby & offer very little resistance
to blood
flow.
b. Lt. ventricle walls are thicker because they
pump blood
through the
body where the resistance to blood flow is
greater.
F.
Operation of the Heart Valves
1. Valves open & close in response to
pressure changes as the
heart contracts &
relaxes
2. Atrioventricular (AV) valves prevent blood
flow from the
ventricles back into the
atria
a. Tricuspid valve on right & bicuspid (or
mitral) on left
b. Backflow is prevented by the contraction of
___________
___________________
tightening the _________________
_____________________
which prevent the valve cusps
from everting
3. Semilunar (SL) valves allow ejection of blood
from the heart into
arteries but prevent
backflow of blood into the ventricles.
a. SL valves open when pressure in the
ventricles exceeds
the pressure
in the arteries
1)
When the ventricles relax, blood flows back from
the
arteries, filling the cusps of the SL valves &
forcing
them to close
G.
__________________________________________: blood supply to
cardiac muscles: coronary arteries
start at base of ascending aorta
1.
right and left coronary arteries supply oxygen & nutrients to
myocardium
2.
cardiac veins (great cardiac vein, middle cardiac vein, & small
cardiac vein) return
blood to the coronary sinus
II. Circulation of Blood
A.
_____________________ circuit:
to lungs for O2/CO2 exchange: right
side of the heart
B.
_____________________ circuit:
to the body: left side of the heart
C.
_____________________: carry blood away from the heart
D.
_____________________: give
blood back to the heart
E.
_____________________: exchanges gases, nutrients & wastes with
the tissues
III. Histology of myocardium (cardiac muscle)
A.
Cardiac muscles have the same arrangement of actin & myosin, &
the
same bands, zones & z discs as
skeletal muscles
B.
They form 2 separate functional networks in the heart; the atrial &
ventricular networks
C.
Fibers within the networks are connected by intercalated discs that
allow them to work together so that
each network serves as a functional
unit
D.
Differences between cardiac and skeletal muscle
1. Compared to skeletal muscle fibers, cardiac
muscle fibers are
shorter in length,
larger in diameter, and squarish rather than
circular in transverse
section. They also exhibit branching.
2. Cardiac fibers have less sarcoplasmic
reticulum & require
_____________________ from extracellular fluid for
contraction
3. All or None law – in skeletal muscles,
impulses are not spread
cell to cell; in cardiac
muscle, they are.
4. Means of stimulation; skeletal muscles
require nerve stimulation.
Cardiac muscles are
_____________________ (initiate their own
action potential)
5. Length of absolute refractory period - lasts
250 msec in cardiac
muscle cells, almost as
long as the contraction; only 1-2 msec in
skeletal muscle. Prevents heart from having tetanic
contractions.
IV. Heart Physiology
A.
_____________________: atria pump together, then ventricles
B.
Electrical Events – intrinsic to the heart (a property of the heart
& not
provided by the nervous system)
1. Intrinsic
Conduction System of the heart - composed of
noncontractile
cardiac cells which initiate and conduct electrical
impulses throughout the
heart. Conduction system allows the
entire heart to beat
faster than it otherwise would because it would
have to rely on cell to
cell transmission of action potential.
(Isolated
heart fibers would beat
at _____________________)
a. Action potential generated by auto rhythmic
cells –
specialized
cells which do no maintain a stable resting
potential;
instead it is unstable and slowly depolarizes to
threshold
where it will fire (all or none) and repolarizes.
b. Heart will continue to beat even if removed
from the body
c. Pacemaker potentials - initiate the action
potentials which
spread
sequentially throughout the heart to
produce the
contractions.
d. Sequence of excitation
1) _______________________________________ –
pacemaker. Cardiac action potential travels
throughout
the atrial myocardium
a) Has a normal rate of ~ 70-75 bpm (with
neural
& hormonal influences); w/o influences
beats
at _________. Excitation spreads to…
2) _______________________________________ –
located
in inferior portion of interatrial speptum, just
above
tricuspid valve. Action potential is
delayed
here
for about ________________ due to smaller
fibers. Allows atria to completely contract before
ventricular
contraction begins. Excitation spreads
to…
3) ________________________________________
(Bundle of His) – the ONLY electrical connection
between
the atria and ventricles. The AV bundle
then
branches
into 2…
4) _______________________________________–
left
and right, one for each ventricle. Each
branch
moves
down the interventricular septum toward the
apex. Smaller fibers branch off which are known as…
5) _______________________________________ –
penetrate
into myocardium throughout the ventricles
&
into papillary muscles
2. Extrinsic innervation of the heart –
autonomic nervous system
control
a. Cardioacceleratory
center – _____________________
neurons from
T1 – T5 region. Innervates SA node, AV
node,
&
ventricle myocardium
b. Cardioinhibitory
center – _____________________
nervous from
vagus nerve.
Innervates SA node & AV node.
c. baroreceptors and chemoreceptors monitor
changes in
blood
pressure and oxygen and carbon dioxide
3. __________________________ – ECG or EKG – measures
the electrical activity
of the heart.
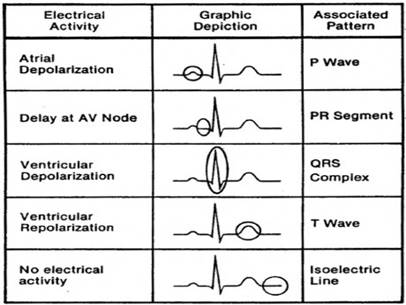
a. _____________________ – atrial
depolarization; spread
of impulse
from SA node over atria (0.08 sec)
b. _____________________ – ventrical
depolarization;
spread of
impulse through ventricles, follows about 0.1 sec
after SA
depolarization begins
c. _____________________ – ventricles are
repolarizing
d.
_____________________ – where atria repolarize
e. _____________________ – ventricles contract
and
empty
f. _____________________ – ventricles relax and
fill
C.
Mechanical events – the _____________________
1. A cardiac cycle consists of
_____________________
(contraction) and
_____________________ (relaxation) of both
atria, rapidly followed
by systole and diastole of both ventricles
2. The phases of the cardiac cycle are…
a) the
relaxation (or quiescent) period: Early
diastole
b)
ventricular filling: Mid to Late diastole, and
c)
ventricular systole: Systole
3. The act of listening to sounds within the
body is called
_____________________,
& it is usually done with a
_____________________
a) The sound
of the heartbeat comes primarily from the
_____________________
in blood flow caused by the
closure of
the valves, not from the contraction of the heart
muscle or
the closing of the valves themselves.
b) The first heart sound (_____________________)
is
created by
blood turbulence associated with the closing of
the
_____________________ soon after ventricular systole
begins.
d) The
second heart sound (_____________________)
represents
the closing of the _____________________ near
the end of
the ventricular systole
c)
The pause between the sounds is the
_____________________
D.
_____________________ (CO) =
amount of blood pumped per minute
1. CO = SV (_________________) X HR
(___________________)
2. Stroke
volume = the volume of blood ejected by the ventricle
with each contraction,
usually _________________ per heartbeat.
a) Three
factors regulate stroke volume:
1)
_____________________, the degree of stretch in
the
heart before it contracts
2)
_____________________, the forcefulness of
contraction
of individual ventricular muscle fibers
3)
_____________________, the pressure that must
be
exceeded if ejection of blood from the ventricles is
to
occur
b) Preload: Effect of stretching
1)
Frank-Starling law of the heart – a
greater
preload
(stretch) on cardiac muscle fibers just before
they
contract increases their force of contraction
during
systole.
2)
Frank-Starling Law equalizes the output of the right
&
left ventricles & keeps the same volume of blood
flowing
to both the systemic and pulmonary
circulations
c) Contractility – the strength of
contraction at any given
preload, is
affected by positive & negative inotropic agents
1)
Increased strength of contraction is caused by
________
influx from extracellular fluid into cytoplasm
a) Caused by increased ________________
stimulation
of the heart à
release of
_____________________
&
_____________________
à an increase
in
_____________________
b)
Also influenced by glucagon, TH, Ca++, and
certain
drugs (like digitalis)
c)
positive inotropic agents increase
contractility
2)
Negative inotropic agents decrease strength of
contraction
a)
acidosis (H+), rising K+, & Ca++ channel
blockers
d) Afterload
– the pressure that must be overcome before a
semilunar
valve can open
1)
_____________________ is usually 80 mmHg
from
the aorta & pulmonary trunk
2) _____________________ (high blood
pressure)
causes
backpressure that is too high & the ventricles
can’t
contract sufficiently to eject a suitable volume of
blood
3. Heart rate – changing heart rate is the
body’s principle
mechanism of short-term
control over cardiac output and blood
pressure.
a) Several factors contribute to regulation of
heart rate
1)
Autonomic nervous system control stems from the
cardiovascular
center in the ___________________
_____________________
a)
sympathetic increases heart rate and force
of
contraction
b)
parasympathetic decreases heart rate
2)
Hormones
a)
epinephrine and norepinephrine quickly
raise
HR, but effect is brief
b)
thyroxine raises HR but more slowly & with
longer
lasting effects
c)
TH enhances effects of epinephrine &
norepinephrine;
therefore prolonged
hyperthyroidism
results in a weakened heart
3) Ions
a)
hypocalcemia (Ca++)à depression of heart
b)
hypercalcemia à
increases excitation &
prolongs
contraction
c)
hypernaturemia (Na+) à inhibits transport of
Ca++
into cells, blocking contraction
d)
hyperkalemia (K+) à interferes with
depolarization
by lowering the resting potential
(results
in heart block & cardiac arrest)
e)
hypokalemia à
heart beats feebly &
abnormal
rhythms
4) Other factors – heart rate decreases with age
& is
lower
in males than in females;
HR increases when
body
temperature is warm & decreases when it is low.
V. Disorders & Homeostatic Imbalances
A.
_____________________, an irregularity in heart rhythm
1. _____________________: > 100 beats/min.
2. _____________________: < 50 beats/min.
3. _____________________: rapid contractions
4. __________________________________________ -
the
appearance
of a second "pacemaker" within the conductance
system
and it tries to override the SA node and can result in the
appearance
of an additional beat (extrasystole)
Sometimes
brought on by the use of too much caffeine or nicotine
B.
____________________________:
sounds in addition to “lubb dupp”
resulting from blood leaks through
heart valves
C.
Strep infections can lead to _____________________ resulting in scar
tissue forming on valves
D.
_____________________ – narrowing of valves resulting in blood
rushing through
E.
__________________________________________: heart doesn't
pump enough blood, retains fluid,
blood backs up in pulmonary circuit, can
lead to pulmonary edema
F.
__________________________________________ (CAD):
degenerative changes in coronary
circulation deprive heart muscle of
oxygen
1. Leading cause of death in the
2. _____________________ –fatty substances
accumulate in the
walls
of the medium-sized & large arteries due to stimuli such as
endothelial
damage
3. _____________________: blockage of coronary
arteries, often
by plaque
4. _____________________: heart pain often with exertion
5. _____________________ – heart attack due to
blood clot
a.
myocardial _____________________ heart attacks kill
heart tissue
6. Treatment options
a.
balloon angioplasty: enlarge arteries, pushes plaque
aside
b.
coronary bypass: bypass blocked arteries